Screening and outcomes of co-occurring traumatic brain injury among people with spinal cord injury
Dr Deborah Snell
Session Information
Traumatic brain injury (TBI) is common among people who sustain traumatic spinal cord injury (tSCI) although rates vary. Co-occurring TBI has been associated with increased length and cost of tSCI rehabilitation, smaller gains from admission to discharge and added difficulties with adjustment and return to productivity. The real impacts are difficult to quantify because TBI is not routinely screened for and is often missed. This means rates in Aotearoa New Zealand (NZ) are unknown. The objectives of this study were to i) Understand the evidence for screening for co-occurring TBI among people with tSCI, and ii) Evaluate utility of TBI screening approaches in the SCI clinical setting.
Abstract
Methods:
For objective i) we conducted a scoping review of relevant literature to synthesise existing knowledge on screening for co-occurring TBI among persons with tSCI.
For Objective ii) a series of consultation hui were undertaken with clinical teams at the Auckland Spinal Rehabilitation Unit, the Burwood Spinal Unit in Christchurch and Medical teams from both units. The purpose of consultation was to find out what stakeholders felt would improve consistency of capturing co-occurring TBI and to better understand clinical challenges for screening for TBI. Then we piloted a brain injury screening tool called the BIST to identify utility of such tools for improving TBI capture among people with tSCI. We also administered a brief cognitive screen and a measure of vestibular and oculomotor markers to determine if these tools improved TBI case ascertainment.
Results:
Objective i) Twenty-five studies were included in the scoping review. We found that screening under-estimated incidence of TBI when approaches relied on a small number of inconsistently collected TBI indicators, especially for mild TBI. Although mixed across studies, outcomes among persons with especially moderate to severe TBI, appeared poorer than those with SCI alone.
Objective ii) Four key themes emerged from consultation hui. These were ‘Non specificity of TBI symptoms’, ‘Timing of TBI screening’, ‘Process for capturing TBI’, and ‘Barriers to capturing TBI’. In the pilot, participants were predominantly male (n = 6), mean age 64 years, and had sustained transport related injuries. Two had a documented TBI diagnosis sustained at the time of their SCI but all met TBI criteria when clinical notes were reviewed for multiple TBI markers. Participants noted difficulty being able to separate their symptom experiences from the impacts of the SCI and/or being an inpatient in hospital, and seemed reluctant to acknowledge the co-occurring TBI.
Conclusions and implications:
- There is a complex interaction between TBI and SCI, and key research gaps for TBIs in mild-moderate range of severity, in particular.
- Consideration of TBI needs to be a routine step in the rehabilitation pathway and incorporated into goal setting.
- A multivariable approach, triangulating acute TBI markers appears most helpful in identifying and confirming TBI. Occupational therapists seem best placed to screen for TBI, bearing in mind limitations of screening tools.
- Further work is needed to understand the impacts of being given a TBI diagnosis after SCI from the person with SCI’s perspective.
Utility of a psychological screening tool early after mild traumatic brain injury
Dr Deborah Snell
Session Information
Psychological difficulties after mild traumatic brain injury (mTBI) are common and can have a profound impact on recovery. Efficiently screening for such factors early after referral to health services can help to direct treatment where it is needed most. Notably though psychologists are a scarce resource and waiting times can be drawn out. A major barrier to assessing psychological factors in clinical practice is that measuring relevant constructs requires a lengthy battery of questionnaires. In our research we modified a brief risk screening tool validated in the pain literature. We then evaluated this tool, which we called the STarT-C, in two prospective mTBI cohorts. We found it was predictive of persistent symptoms and disability six-nine months after injury in adults with a recent mTBI attending an Emergency Department in Canada, as well as those seeking outpatient treatment at an mTBI clinic in New Zealand (NZ). It was also just as good at predicting post-concussion symptom outcomes as a full battery of questionnaires assessing STarT-C content.
Abstract
The objective of our current study was to evaluate the utility of the STarT-C in NZ concussion services. We were interested in how well STarT-C risk categories matched other indicators of risk such as symptom burden and psychology referral needs, as well as clinician experiences with the tool.
Methods:
This is a small mixed methods pilot study evaluating the utility of the STarT-C in two concussion services in NZ, one located in a large North Island centre (site 1) and one in central South Island (site 2). The quantitative component of the study was an audit of consecutive referrals triaged by the concussion teams following introduction of the STarT-C. The qualitative component involved semi-structured interviews with triaging clinicians to better understand their experiences of using the tool.
Results:
The patient sample included n = 112 consecutive referrals (site 1, mean age 39 years, 44% male) and n = 51 referrals (site 2, mean age 36 years, 43% male). The clinician sample included physiotherapists (n = 2) and occupational therapists (n = 3). In the quantitative audit STarT-C risk categories correlated with a widely used symptom tool called the Brain Injury Screening Tool (BIST). In the qualitative interviews clinicians felt the tool helped them prioritize who needed referral to a psychologist right away versus who could be monitored vs those unlikely to need psychology. It helped them reduce their waiting list for psychology input. It helped them start a conversation about psychological symptoms, ask questions they might not have routinely asked, and focused multi-disciplinary team discussion.
Conclusions and implications:
The STarT-C may be a useful brief screening tool in multi-disciplinary concussion services to determine risk and clinical need. The tool may be useful for identifying those at risk of prolonged recovery who may benefit from early psychological support. Our programme of work validating the STarT-C and proposed further refinements are ongoing.
Acceptance and Commitment Therapy for Mild Traumatic Brain Injury (ACTion mTBI): Feasibility Study of Effectiveness
Dr Josh Faulkner
Session Information
Psychological factors are well known to influence recovery following mild traumatic brain injury (mTBI). Psychological interventions can therefore be helpful for this population. Acceptance and Commitment Therapy (ACT) is a world-renowned psychotherapy, yet its effectiveness in mTBI is limited. To address this, we have developed ACTion mTBI, a 5-session, ACT-informed intervention that incorporates all six processes of the ACT hexaflex for a mTBI recovery context. This study examines the feasibility of ACTion mTBI using quantitative and qualitative methods when compared to a CBT intervention.
Abstract
Background and Objectives: Psychological factors are well known to influence recovery following mild traumatic brain injury (mTBI). Psychological interventions can therefore be helpful for this population. Acceptance and Commitment Therapy (ACT) is a world-renowned psychotherapy, yet its effectiveness in mTBI is limited. To address this, we have developed ACTion mTBI, a 5-session, ACT-informed intervention that incorporates all six processes of the ACT hexaflex for a mTBI recovery context. This study examines the feasibility of ACTion mTBI using quantitative and qualitative methods when compared to a CBT intervention.
Method: This study was embedded within community-based multidisciplinary rehabilitation services in New Zealand. Using site randomisation, 24 participants respectively engaged in either ACTion mTBI or CBT.
Results: The ACTion mTBI group showed a significantly greater reduction in post-concussion symptoms, psychological distress and functional disability when compared to the CBT group at post-treatment evaluations. ACTion mTBI also had a significant increase in psychological flexibility. Thematic analysis of post-treatment interviews for the ACTion mTBI group revealed the following themes 1). attacking the concussion from a different direction 2). a positive impact on recovery, 3). helpful aspects of the intervention and 4). enablers of intervention effectiveness.
Conclusions: This study illustrates the potential of ACT as a psychotherapy for mTBI and sheds light on the specific aspects of this approach that may be beneficial for this population.
Correspondence: Josh W Faulkner, josh.faulkner@vuw.ac.nz
An exploration of families’ lived experiences of attention-related communication difficulties following traumatic brain injury
Dr Maegan VanSolkema
Session Information
To explore families’ experiences of living with someone who has attention and communication difficulties following a traumatic brain injury (TBI). Attention-related communication difficulties are common following TBI, but to date there is limited research into the effects on the family with respect to this cognitive communication difficulty (CCD).
Abstract
Introduction/Purpose: To explore families’ experiences of living with someone who has attention and communication difficulties following a traumatic brain injury (TBI). Attention-related communication difficulties are common following TBI, but to date there is limited research into the effects on the family with respect to this cognitive communication difficulty (CCD).
Methods: Recruitment of family members was completed through TBI community rehabilitation services. Inclusion criteria were the family member needed to be living with an individual who had sustained a moderate-severe TBI at least 6 months prior to the study with self-reported attention and communication difficulties. A semi-structured interview was completed. Qualitative interview data underwent reflexive thematic analysis with an inductive approach.
Results: 11 family members (including wives, mothers, a father, and a daughter) were interviewed. Two themes were generated that explored the lived experiences of the family. The first, adjustment to the new normal, outlines the changes and adaptations the families made to live and support their loved one’s attention and communication difficulties. The second theme, the load the family carries, reviews the two polarities of facilitation and support along with the burden the family endure following the injury.
Conclusion: The themes outline how attention-related communication difficulties following TBI bring additional burden and challenges for family for years following the injury. Family report adapting their social lives and have learned to implement specific strategies to improve their person’s ability to interact and participate in conversations. Clinical implications will be discussed.
Learning Outcomes: To understand and define attention-related communication difficulties. Also, to understand the impact of attention-related communication difficulties have both on the person with TBI and how their family manages these years following the injury. Recommendations and clinical implications related to integrating family system therapy and focus as part of the rehabilitation team.
From grief to growth, Tori’s story
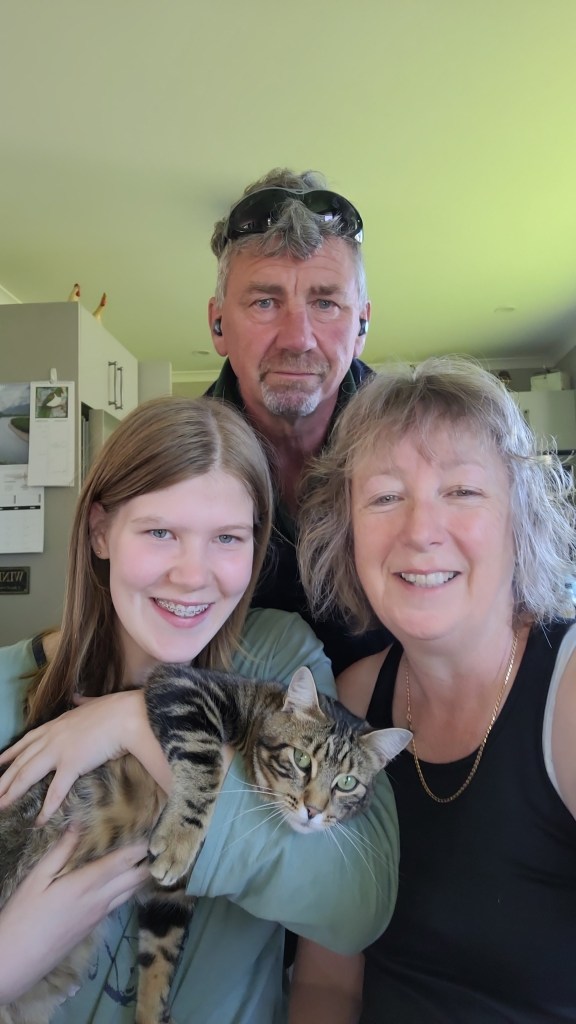
Neeka Aicken, Sandra Johnstone
Session Information
Tori’s life started from a place of grief. She was born to a mother who chose Tori’s life over her own. As sad as that is, the following 17 years have proved that you should never give up hope (which is also her middle name).
Abstract
Tori’s life started from a place of grief. She was born to a mother who chose Tori’s life over her own. As sad as that is, the following 17 years have proved that you should never give up hope (which is also her middle name).
Tori sustained a traumatic brain injury in utero as a result of radiation exposure while her mother was undergoing investigations and subsequent treatments for cancer while unknowingly pregnant. Following many assessments and opinions Tori is now diagnosed to have an acquired diffuse brain injury secondary to radiation, cortical dysplasia with heterotopia and intellectual disability.
As a team including family, her rehabilitation therapists, school and community we have to regularly evolve and adapt as Tori needs us to. There is no blueprint or manual for us to follow for her type of injury.
Tori has taught us not to place limits on her ability to achieve. Everything she has achieved in life has been hard fought but through holistic support, repetition and consistency she has developed an incredible work ethic and has had some great successes.
Now age 17, Tori’s trajectory of meeting developmental milestones have been unpredictable and variable. As she grows into a young woman with a view to live in her own tiny home in the future, we are needing to support Tori to develop the skills to enable this and consider what supports she will need to live independently and safely in her local community. Her Dad and step-mum have had many moments of scratching their heads but have been appreciative of the access to a team of professionals to seek guidance from and will share their insights of parenting Tori. Tori’s education has required an adapted curriculum to support her learning, and her school and rehabilitation team work closely to support access to education.
Our presentation will aim to share stories from all perspectives of Tori’s rehabilitation journey so far with its challenges and successes along the way.
“His moment of misfortune, my years of learnings”: A personal insight into life skills coaching a young adult with TBI
Mr Alan Signal
Session Information
AbStract
In my presentation, I will introduce you to Andrew. With his consent, I am sharing our journey. A journey which has focused on his independence, my coaching, his growth, my learnings and the need for a more social – rather than clinical – method of managing TBI’s within the ACC framework.
Eight years ago, I met Andrew, a 31-year old adult male with TBI, living at home with his parents. Andrew’s life was significantly different than what he dreamed of as a teenager. A moment of misfortune he calls his accident with a train, a moment which for the next decade kept him perpetually aged 17 years old. He was very keen to please, a “yes-man” you could say. I focused on identifying what his goals and aspirations were, but I was met with his parents’ goals and aspirations instead. Getting Andrew away from his parents provided him with the space to enable him to voice his goals. Quite simply, Andrew wanted to be independent, have his own friends and be empowered to make his own decisions around his life.
It is well recognised that rehabilitation focuses on optimising independence through skill acquisition across behaviour, self-care, living skills, social integration, communication and relationships. For me and my experiences with Andrew it is the journey to achieving these skills which is the measure of success, not necessarily the arrival at certain pre-determined outcomes. It is here that the ACC rehabilitation framework and I diverge. For me, clients with TBI will always be a work-in-progress, as their recovery will always vary.
As a Rehabilitation Coach for Laura Fergusson Trust in Wellington, my challenge was to help Andrew identify life goals and work together to develop his skills and knowledge for him to better achieve these within the ACC Living my Life framework. As a practitioner working within this framework, I have found that TBI rehabilitation based on a return-to-work principle as opposed to a focus on increasing independent living skills within the home and social settings of people does not always achieve the best outcome for a client. For a young person like Andrew, there is no “return-to” anywhere, as he had yet achieve any life milestones.
My role has been to help Andrew identify and develop the skill sets he has needed to navigate this journey. I have also learnt a lot about myself and how reflection on my personal lived experiences has allowed me to be a better coach for Andrew. I have now started working with Nicky, Andrew’s wife, helping her upskill so I can soon pass on the baton to her, so she can continue to support and guide Andrew on his journey.
In sharing the journey, I will touch upon some key issues which impact upon the life of a person with TBI: managing expectations around recovery and developmental milestones; rebuilding social connections; emotional regulation; and creating new relationships with intimate partners and developing a community of support.
Traumatic Brain Injury and Aphasia: Pre-vocational and Vocational Rehabilitation Pathways integrating Cognitive Neuroscience informed through Lived Experience.
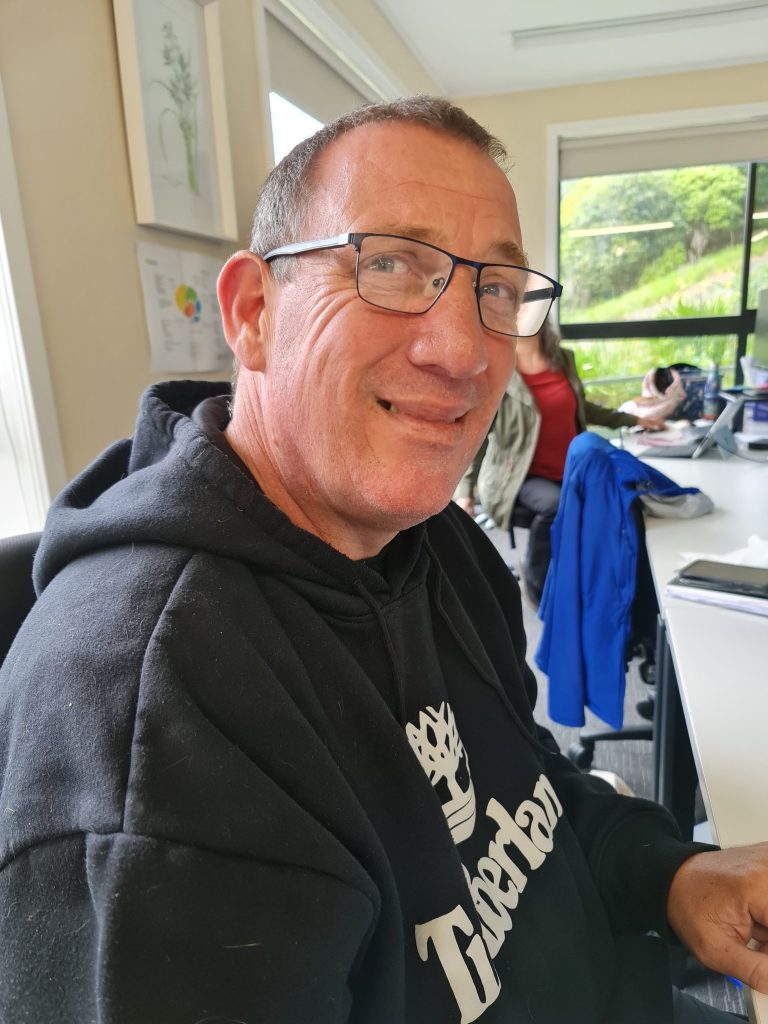
Mr Garry Whittaker
Session Information
This session intends to demonstrate how a noval approach has been applied from the perspective of an individual with a lived brain injury experience to strengthen rehabilitation and recovery enhancing pre-vocational and vocational outcomes for individuals where cognitive skills are impacted through aphasia.
AbStract
This proposed session aims to provide an insight into the unique pre-vocational and vocational rehabilitation strategy adopted and integrated with existing clinical practices to support return to work following a Traumatic Brain Injury occurring in February 2020. The rehabilitation strategy included a personally initiated training program utilising an evidence-based cognitive computerised brain training routine based on the principles of neuroplasticity, informal learning and a physical fitness routine. Amongst the research literature focused on vocational outcomes, Graham et al. (2011) found that people with aphasia had inferior re-employment rates (28%) when compared to acquired brain injury survivors (44%) aged between 16-65.
This session intends to demonstrate how a noval approach has been applied from the perspective of an individual with a lived brain injury experience to strengthen rehabilitation and recovery enhancing pre-vocational and vocational outcomes for individuals where cognitive skills are impacted through aphasia.
The Acquired Brain Injury suspected to have occurred through an assault generated a large left frontotemporal intraparenchymal haemorrhage with marked midline shift and a right temporal extradural haematoma with associated moderate local mass effect as well as a fracture of the right parietal bone. The neurological repercussion of the injury included significant receptive aphasia, moderate expressive aphasia and anomic aphasia as well as Post Traumatic Amnesia.
Clinical assessment highlighted marked differences in confrontation naming and word-finding which would significantly undermine the cognitive capabilities required to return to work successfully as the Regional Manager with Training Services within the Education and Skills Reform division of the NSW Department of Education. Standard clinical practices were applied to ameliorate the neurological language deficits acquired through the brain injury.
The guided intervention and support included occupational therapy and speech pathology with the latter focused on activities targeting phonemic and semantic fluency improvements. During the rehabilitation an additional strategy was individually initiated and tailored to include a brain plasticity-based computerised cognitive training program.
The Brain HQ program was developed by Posit Science whose co-founder Dr. Michael Merzenich has been a leading pioneer in brain plasticity research for nearly five decades. The web-based learning program utilises training tools designed to rejuvenate brain function by driving changes in eight key areas including aural speech and language. This element of the rehabilitation process applied the key neuroplasticity principles of repetition and intensity. The adoption of strategies personally initiated and applied in addition to the accepted clinical practice throughout the pre-vocational and vocational rehabilitation period and beyond, particularly for ongoing cognitive health, have been foundational in enabling a successful recovery from the injury and return to work as the Regional Manager.
Rejuvenation through this lived experience has generated a personal passion for advocacy to raise awareness about our own brain wellbeing and the need to incorporate brain fitness into our everyday living to maintain and enhance our cognitive health integrated with our nutritional, aerobic and cardiovascular exercise routines.
A Tale of Two Perspectives: From Nurse to Patient and Innocent Until Proven Guilty
Mrs Sarah Raffell, Miss Tori Dent
Session Information
AbSTract
Tori’s life was full; Twenty-five years old, a nurse, an avid and health and fitness enthusiast, the life of the party, a global traveller, a dog Mum, a sibling to 4 and a twin. All of this changed when an undifferentiated brainstem lesion decided her body was to be its home. With determination, sass, tenacity and leaning on her healthcare knowledge, she embarked on a journey that defied expectations and achieved the improbable to create a new life, one that is also full albeit very different to what she imagined.
Tori was told that she would not eat or drink again, and that a PEG would be the mode in which she would get her nutrients. She was told she would not speak clearly and that she would likely need a device to help her be understood. She was told she could not live independently and after years of having lived alone she was forced to conder a life of dependence. It was insinuated that her mobility wouldn’t progress she would need a wheelchair. She had to sign risk feeding documents. It was a continual battle between what she felt possible and what imaging showed and what she was told was impossible.
Given she was a perioperative nurse and had spent years studying and working in the healthcare sector, this was a stark contrast to how she perceived healthcare and rehab should be. She didn’t want to be a rehab patient in bed. She didn’t want to listen to the goals that were set for her – they were so safe, so risk adverse and they seemed be for the staff and not for her. She wanted to be heard. She wanted to have a voice, and it felt like she didn’t have one. If she was to push herself anyway, isn’t the hospital the best place to do this?
Enter a Speech Pathologist who saw a nurse with extensive knowledge, an advocate for herself and someone who didn’t fit the mould of being cognitively impaired. A handover was given that was so incongruent with the patient in front of her and seemed at odds with the goals this patient clearly wanted to achieve. This patient had to continuously prove to the staff that she was able, was capable and that she knew her boundaries. Thus began a rehabilitation journey of pushing limits and battling fears that stemmed more from subjective perceptions than solid clinical evidence.
This is the tale of the two perspectives; one from a nurse who became nursed, and one from a speech pathologist who fought to shift conceptions of risk in a sub-acute rehabilitation setting.
This is the story of Tori Dent and her recovery from a brain injury.
Efficacy of GameBreaker Softshell Headgear in Mitigating Brain Injury Risk: Reducing Linear and Rotational Forces During Controlled Drop Tests
Mrs Annette Swale
Session Information
AbStract
Affiliations
¹ Department of Mechanical Engineering, University of Canterbury, Christchurch, New Zealand
² School of Health Sciences, University of Canterbury, Christchurch, New Zealand
Purpose:
This study aimed to evaluate the effectiveness of two types of softshell headgear, GameBreaker-Pro and GameBreaker-Prototype, in reducing peak linear acceleration (PLA), peak rotational acceleration (PRA), and peak rotational velocity (PRV) during controlled drop tests. These headgear models differ in thickness and were tested for their ability to mitigate impact forces, which are linked to brain injuries in contact sports like rugby. Given the increasing awareness of traumatic brain injuries (TBI) and concussions in youth sports, this study contributes to the growing body of research exploring protective measures that may reduce the risk of such injuries.
Methods:
The headgear was subjected to drop tests from heights of 15 cm, 30 cm, 45 cm, and 60 cm, with impacts applied at five orientations: forehead, front boss, rear boss, rear, and side. The Hybrid III 50th percentile headform was fitted with accelerometers to record PLA, PRA, and PRV. These metrics were used to evaluate the capacity of the headgear to attenuate impact forces compared to a no-headgear baseline.
Results:
Both GameBreaker-Pro and GameBreaker-Prototype significantly reduced PLA, PRA, and PRV compared to no headgear. GameBreaker-Pro reduced PLA by up to 44.9% (side orientation) and 34.4% (rear orientation), while PRA reductions reached 52.1% (forehead orientation) and 38.5% (front boss orientation). Similarly, GameBreaker-Prototype demonstrated strong performance, with PLA reductions of up to 41.2% (side orientation) and 34.1% (rear orientation). PRA reductions were also significant, with a maximum reduction of 49.2% (forehead orientation) and 40.2% reduction (rear orientation). Composite percentage reductions in PRV ranged from 27.4% to 28.4%, showing moderate effectiveness in attenuating rotational velocities. The composite performance of both headgear types suggests they provide substantial protection in high-impact scenarios.
Conclusions:
This study highlights the potential of GameBreaker softshell headgear to mitigate head impact forces, outperforming the no headgear condition and current World Rugby Law 4-approved headgear in reducing PLA, PRA, and PRV. GameBreaker-Pro, with its thicker foam structure, performed particularly well in absorbing both linear and rotational forces, which are key contributors to the risk of traumatic brain injuries. These results emphasise the importance of using advanced headgear in contact sports to reduce the intensity of impacts, thereby potentially lowering the incidence of concussions and other brain injuries. The findings suggest a need for further refinement in headgear design and materials, as well as a reconsideration of current headgear regulations to prioritise player safety.
Keywords:
Headgear, Rugby, Head Injury, Brain Injuries, Traumatic Brain Injuries, Concussion
Creating Better Outcomes by Removing Digital Interface Barriers
Dr Chandra Harrison
Session Information
This session will identify some of the main barriers for people with TBI, explore how to remove those barriers and discuss how well-designed digital solutions such as AI can support people with TBI. The session aims to raise awareness for everyone, offer some basic tools to fix the barriers if you can and encourage all attendees to call out the barriers whenever they can.
AbStract
As more and more of our everyday lives involve digital interaction, the greater the need to remove digital barriers becomes apparent. We are all being pushed to transact online, whether it is finding a date or finding employment. With the introduction of Artificial Intelligence based systems the digital space has increased even further.
But digital interfaces often present huge barriers to users of all types including those with TBI. These barriers might stop people from purchasing or participating, or even worse increase the risks of digital misadventure. The way systems are designed, the way the content is written, the way the solution is coded, the passwords and multi-factor authentication requirements can all impact on the user experience.
Designing more inclusive digital systems that allow users to interact in a way that suits their needs creates better outcomes for the users, and better outcomes for the owners of the digital systems. For example, an employment website that is overly complex and cumbersome or can’t be accessed using assistive technology presents a significant barrier to people with TBI seeking employment. In addition, employers are potentially missing out on wonderful candidates because they aren’t able to apply for the jobs, and the organisation is missing out on the benefits of having a more diverse workforce.
This session will identify some of the main barriers for people with TBI, explore how to remove those barriers and discuss how well-designed digital solutions such as AI can support people with TBI. The session aims to raise awareness for everyone, offer some basic tools to fix the barriers if you can and encourage all attendees to call out the barriers whenever they can.
Creating re-connection for people with long-term disability following traumatic brain injury
Anneke Duyvestyn & Kirsty MacDonald
Session Information
Hear about Laura Fergusson Brain Injury Trust’s Living my Life Service and group program, Reconnect, which is ACC’s only long term disability service supporting clients to have choice and control over where they go, what they do, where they live and who with. Hear from Key Workers and Rehab Coaches about the work they do 1:1 and in groups with clients, as well as from clients who receive coaching and participate in our group programs.
AbStract
Evidence-based interdisciplinary rehabilitation: Translating clinical practice guidelines into real world settings
Dr Christine Canty, Dr Warren Cossou
Session Information
We will explore the challenges and practical considerations for engaging in cognitive rehabilitation within the ACC setting. A panel discussion with both therapists and clients will follow. Strategies for ensuring that evidence-based cognitive rehabilitation remains patient-centred and is truly interdisciplinary to maximise benefit will be discussed.
AbStract
The INCOG 2.0 guidelines provide evidence-based recommendations for cognitive rehabilitation with individuals with TBI. This seminar will review recommendations relating to self-monitoring, metacognitive strategy training, and cognitive-communication rehabilitation. Two clinicians, a neuropsychologist and a speech language therapist, will present a clinical case with video excerpts, illustrating application of these guidelines in a community setting for a client with significant cognitive-communication difficulties and executive dysfunction. We will explore the challenges and practical considerations for engaging in cognitive rehabilitation within the ACC setting. A panel discussion with both therapists and clients will follow. Strategies for ensuring that evidence-based cognitive rehabilitation remains patient-centred and is truly interdisciplinary to maximise benefit will be discussed.
Patient-centred interdisciplinary rehabilitation
Sharlie Kennards, Nikki Sainsbury and Dan
Session Information
Two people with traumatic brain injury tell the story of their brain injury recovery and rehabilitation experience. A panel discussion will follow with clients and their therapists, discussing topics related to patient-centred interdisciplinary rehabilitation, including – How do we practice evidence based cognitive rehabilitation while also staying person-centred? How do we ensure that our rehabilitation is truly interdisciplinary? How do we balance insight and hope after brain injury?
AbStract
“Who is this person I am tramping with and where are we going?” Neuropsychological formulation and real-life outcomes
Dr Nic Ward and Dr Siobhan Palmer
Session Information
Think of rehabilitation like a journey, as if we’re going on a tramp together – where are we going, who are we going with, what do we need, how do we approach the steep hills together, and how will we know when we get to the end? Based on the Evans, Wilson et al (2009) model of holistic neuropsychological formulation, this presentation will take you on a journey, providing examples of how we can weave together cognitive-emotional interventions to provide personally meaningful treatment and describe real life outcomes. We will look at applying the formulation model to moderate/ severe brain injury and also to concussion.
AbStract
The use of music therapy with traumatic brain injury clients
Kimberley Wade & Renata Kuswanto
Session Information
Renata and Kimberley from Southern Music Therapy will be presenting about Music Therapy and Neurologic Music Therapy with several TBI Case examples from their clinical practice. We will be discussing how we use live familiar music to help retain orientation information, enhance long term memory, communication, emotional expression, and pain relief. How we utilize the structure and predictability of music along with movement & breathing to promote functional movement and relaxation. Music therapy, particularly through songwriting and therapeutic singing, can enhance communication & emotional expression. Giving examples of the importance of the therapeutic relationship to build meaningful interchangeable communication through these musical experiences. We will also discuss our neurologic music therapy techniques and how we use these to work on functional goals such as sit to stand, arm mobility and at times gentle stretching assist in keeping active. We will also talk about our pathways within our practice from individual work into small and large group work. Discussing groups like the Cantabrainers Choir which is a neurological choir based in Christchurch.